Total Hip Replacement
Understanding Total Hip Replacement
Total hip replacement produces a prosthetic joint that closely approximates normal anatomic functions and is relatively painless. More importantly, it allows a return to activity and a freedom from limitation, restoring quality of life for patients.
Non-operative treatment is effective in the early stages of patients experiencing hip pain. Minimizing weight bearing by using a cane, crutches, or a walker will help improve the discomfort in the joint. Hip pain may also be relieved with the use of anti-inflammatory medication, injections, and/or physical therapy. These interventions may relieve the pain temporarily or in some cases permanently.
What is a total hip replacement?
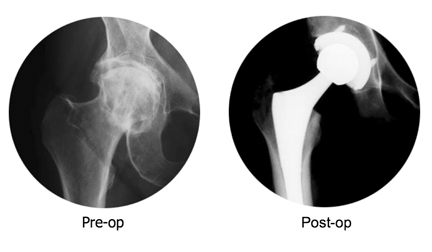
A total hip replacement is a procedure performed for severe arthritis or a severe degenerative condition of the hip joint. It is called a total hip replacement because both the ball and the socket of your hip are resurfaced. The hip replacement is made of a metal (usually titanium or a cobalt/chrome alloy). The ball of the hip replacement is either a metal or a ceramic material. The socket lining is either an ultra high molecular weight polyethylene (a special machined plastic) or a ceramic material. These linings allow for a smooth surface for the ball to rotate in the socket with minimal wear during regular activity.
Who is a candidate for total hip replacement?
Total hip replacement is an elective procedure. It is designed to alleviate the pain from severe arthritis or degenerative conditions of the hip joint. If your history, physical exam, and x-rays reveal that you would get significant relief from the procedure then you are a candidate for total hip replacement. Before proceeding with a total hip replacement, nonoperative means to control your symptoms are generally tried first. Use of pain medication, a cane, activity modification, and possibly injection therapy are examples. If you have tried some or all of these and still have significant pain that interferes with the quality of your life on a daily basis, then you are a candidate for total hip replacement.
If I am a candidate for a total hip replacement, when should I have it done?
Again, a hip replacement is an elective procedure. If you have pain on a daily basis that interferes with the quality of your life despite nonsurgical treatments, then you are a good candidate for the procedure. If this is the case, then you have greater than 95% chance of having significant pain relief from a total hip replacement.
What do I do before surgery?
In general, you will need to be seen by your primary care physician and other medical specialists before surgery for medical clearance. This gives our anesthesiologists and medical personnel important information to best care for you during and after surgery. If your primary care physician practices at our hospital, they will follow your progress with me while you are in the hospital. If your medical doctors do not actively practice at the hospitals that I perform this procedure, then we will ask which medical physician they would prefer to follow your progress while you are in the hospital. You will need preoperative laboratories and tests. You will also be asked if you would like to donate your own blood prior to surgery so that I can give this back to you after your hip replacement is complete. I will provide you with more extensive Total Hip Replacement educational materials during your appointment.
What do I do the day before surgery?
The day before surgery you should not eat or drink anything after midnight. We will instruct you when to come to the hospital before the procedure. It is important to arrive at or before that time so that the nurses can get everything ready for you (including IV placement, preoperative antibiotics, paperwork and skin preparation.
What happens immediately after surgery?
Generally, you will stay in the hospital for three to four days. You are placed on a blood thinner to prevent blood clots. If you donated your own blood, it will be given back to you on the first or second postoperative day. You will also be given antibiotics immediately before and after your surgery to prevent infection.
Immediately after surgery you will rest. On the first postoperative day, you will meet the therapists. They will assist you in walking and transferring from bed to chair, and show you certain exercises to perform and positions that we want you to avoid immediately after hip surgery. You will need a walker after surgery while you regain strength. Once you graduate to a more extensive rehabilitation program, you will be transferred from the regular hospital bed to a rehabilitation unit. Occasionally a patient is walking so well that they bypass the rehab unit and go straight home from the hospital.
What determines whether I can go home or whether I need more rehab?
Depending on how far you are able to walk, how much help you have at home, and the terrain of your home (stairs, etc…) will determine whether you can go home or whether you will need a few days to weeks of rehabilitation. Most people need several days of rehabilitation after their hospital stay to build up their strength enough to feel safe and be safe at home. Rehabilitation may be performed at the hospital or an outside facility. You and your insurance company may determine the exact location as some insurance companies specify certain rehab facilities for your insurance to cover the care. We have clinical nurse specialists who will help assist you in your discharge and rehabilitation planning.
What happens once I’m home?
We recommend that you use your walker for six weeks after the surgery. This gives the hip rest while all the tissues (muscles and tendons) heal. At six weeks we will advance you from a walker to a cane or nothing at all, depending on how much strength you have regained and how you feel without the walker. You will take a blood thinning medication, either coumadin or aspirin, for 6 weeks following surgery to prevent blood clots. You also will need to avoid certain body positions that predispose you to a dislocation of the hip. These will have been reviewed with you extensively while you were in the hospital.
What are the risks of total hip replacement surgery?
As with any surgery, there are specific risks with the Total Hip Replacement procedure. Although uncommon, risks include but are not limited to infection, dislocation, bleeding, thigh pain, limb length inequality, swelling in the leg, medical problems such as blood clots or pneumonia, anesthetic risks, early loosening of the device, wound complications, and damage to nerves or blood vessels.
Want to make an appointment?
Phone: (707) 254-7117
Fill out our intake form so we can set up your visit with the correct doctor.
